MDS-AML Spectrum
Background on MDS and AML
Background on MDS and AML
The MDS-AML Spectrum
The MDS-AML Spectrum
While MDS and AML are both characterized by an excess of myeloblasts and cytopenias, MDS skews toward dysplasia and ineffective hematopoiesis, whereas AML skews toward increased “blasts”.10,11 As the spectrum of disease progresses, stem cells acquire mutations that disrupt the normal formation and differentiation of peripheral blood cells.12,13
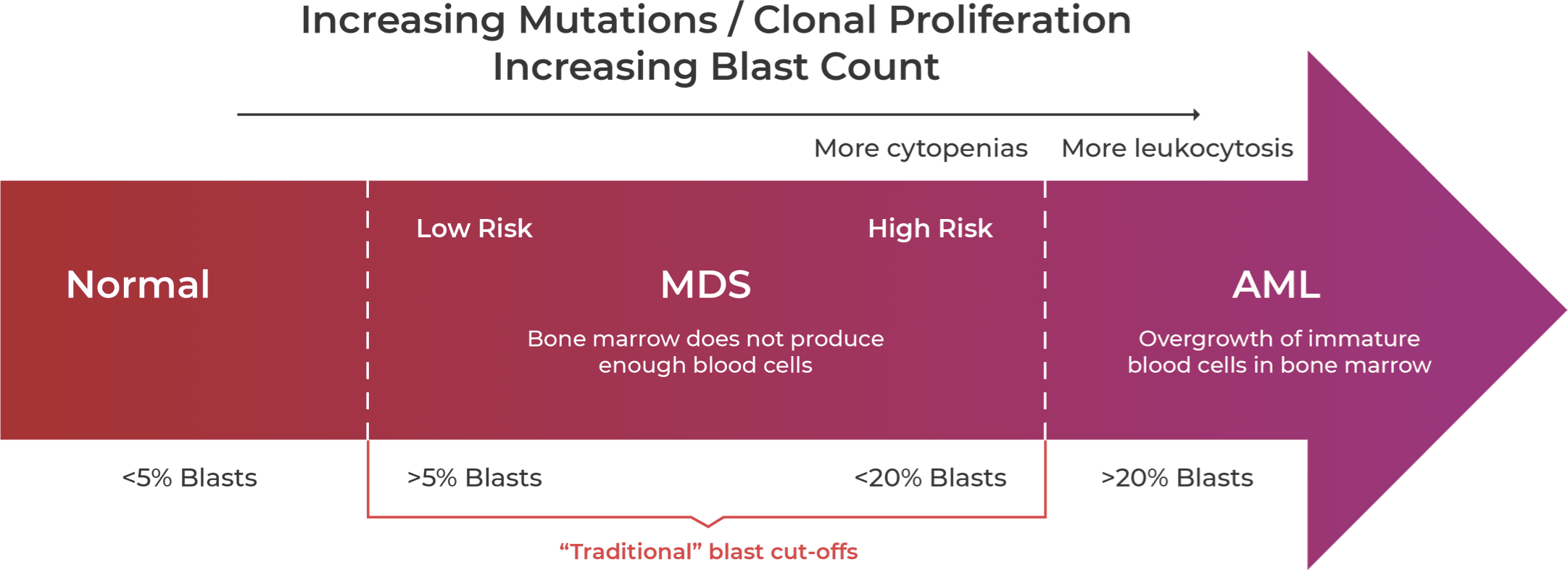
Guidelines are relaxing the traditional blast count cut-offs to suggest MDS-AML is more a spectrum of disease.12,14-18
MDS and AML are now thought to be part of a spectrum of disease, with blast counts increasing as MDS progresses to AML.14 This blast count cutoff is traditionally defined at 20%; however, guidelines are rapidly changing to reflect the overlap of the two related disease states and to take into account mutational status, which may influence risk stratification.15
Updated Guidelines Reflect
MDS-AML Spectrum
Updated Guidelines Reflect MDS-AML Spectrum
Recent changes to the World Health Organization (WHO) and International Consensus Classification (ICC) classifications reflect a move away from morphological definition of disease and toward a genetic basis for defining MDS and AML.15,18,19 The ICC has refined the bone marrow blast categories for MDS from <5% to 9% and created a new MDS/AML category for 10%-19% blasts, whereas the WHO categories of MDS-IB2 and MDS-f retain blast counts up to 19%.15,18 WHO 2022 eliminated blast cutoffs for most AML types with defining genetic alterations but retained a 20% blast cutoff to delineate MDS from AML.15 The lowered ICC 2022 blast cutoff suggests both the relevance of genetic alterations and that MDS-AML is a spectrum of disease.18
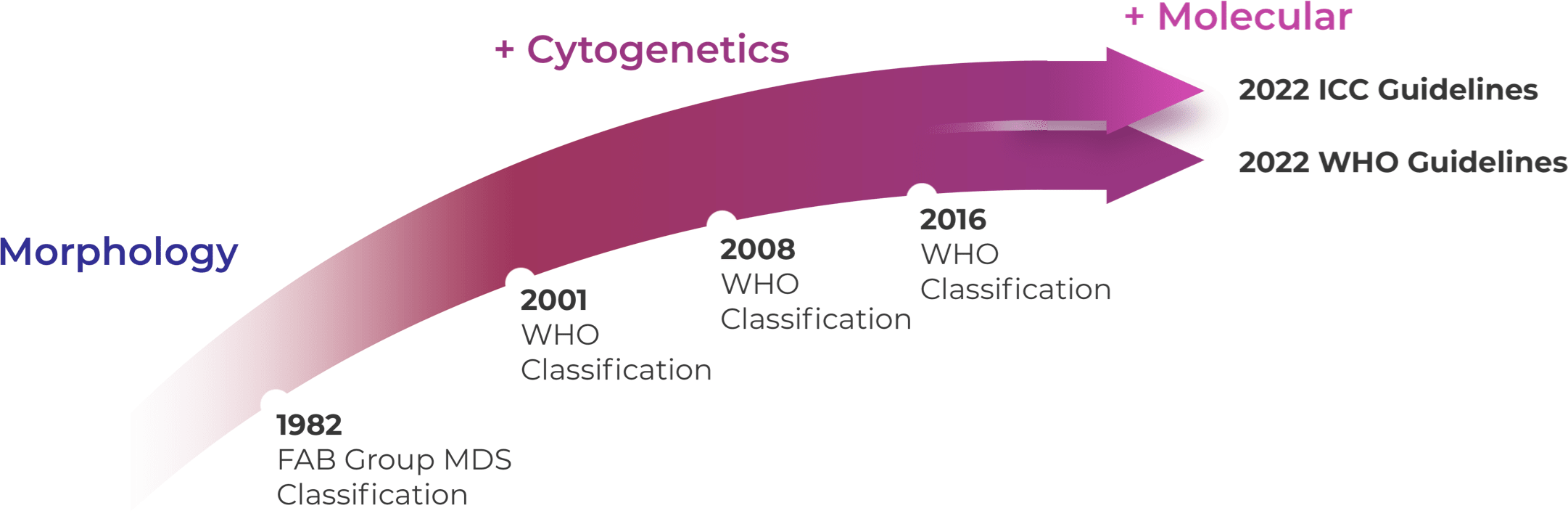
WHO 2016 and prior was mostly based on morphology and cytogenetics.20 WHO 2022 and ICC 2022 reorganized MDS categories by emphasizing histological and genetic co-variates with slightly different blast categories.15,18,21
Genetic Drivers of
MDS and AML
Genetic Drivers of MDS and AML
Mutated IDH, a recurrent genetic driver, may be expressed in both MDS and AML patients as indicated by genetic profiling.13,22
Hematology studies have shed light on the impact of IDH1 mutations in MDS and AML, revealing a poorer prognosis for patients with these mutations compared to those with IDH2 mutations or IDH wild-type.23,24 In MDS, IDH1 mutations are considered early “driver” mutations, occurring in approximately 3.6% of MDS patients.22-25 As the disease progresses from low-risk MDS to high-risk MDS to AML, the frequency of mIDH1 in patient populations increases, indicating its role in disease evolution.25-27
Clinical Crossfire: Expert
Discussion on MDS and AML
Clinical Crossfire: Expert Discussion on MDS and AML
Expert Joshua Zeidner, MD discusses recent updates to the ICC and WHO classification of AML and MDS.
Expert Uma Borate, MD discusses the impact of high-risk mutations on MDS to AML progression.
What additional topics in IDH science
would you like to hear about?
What additional topics in IDH science would you like to hear about?
LearnMore about the prognostic impact of mIDH in MDS and AML LearnMore about the prognostic impact of IDH mutations in GliomaStay in the Know
Keep up to date on the latest in
IDH science from leading experts.
References:
1. Klepin HD, Rao AV, Pardee TS. JCO. 2014;32(24):2541-2552. doi:10.1200/JCO.2014.55.1564 2. Steensma DP. Mayo Clinic Proceedings. 2015;90(7):969-983. doi:10.1016/j.mayocp.2015.04.001 3. American Cancer Society. About MDS website. https://www.cancer.org/content/dam/CRC/PDF/Public/8743.00.pdf. Accessed February 22, 2023. 4. Higgins A, Shah MV. Genes. 2020;11(7):749. doi:10.3390/genes11070749 5. Ye X, Chen D, Zheng Y, Wu C, Zhu X, Huang J. Hematological Oncology. 2019;37(4):438-446. doi:10.1002/hon.2660 6. Montoro J, Vallespi T, Sancho E, et al. Blood. 2011;118(21):5026-5026. doi:10.1182/blood.V118.21.5026.5026 7. Brunner AM, Blonquist TM, Hobbs GS, et al. Blood Advances. 2017;1(23):2032-2040. doi:10.1182/bloodadvances.2017010165 8. Nachtkamp K, Stark R, Strupp C, et al. Ann Hematol. 2016;95(6):937-944. doi:10.1007/s00277-016-2649-3 9. Alonso‐Fernandez‐Gatta M, Martin‐Garcia A, Martin‐Garcia AC, et al. Br J Haematol. 2021;195(4):536-541. doi:10.1111/bjh.17652 10. Chan O, Renneville A, Padron E. Leukemia. 2021;35(6):1552-1562. doi:10.1038/s41375-021-01207-3 11. Mughal TI, Cross NCP, Padron E, et al. Haematologica. 2015;100(9):1117-1130. doi:10.3324/haematol.2014.114660 12. Joudinaud R, Boyer T. Front Oncol. 2021;11:730899. doi:10.3389/fonc.2021.730899 13. Woll PS, Yoshizato T, Hellström‐Lindberg E. J Intern Med. 2022;292(2):262-277. doi:10.1111/joim.13535 14. Ambinder AJ, DeZern AE. Front Oncol. 2022;12:1033534. doi:10.3389/fonc.2022.1033534 15. Khoury JD, Solary E, Abla O, et al. Leukemia. 2022;36(7):1703-1719. doi:10.1038/s41375-022-01613-1 16. Pontrelli G, Loscalzo C, L’Eplattenier M. JAAPA. 2023;36(6):17-21. doi:10.1097/01.JAA.0000931428.87936.72 17. Bewersdorf JP, Zeidan AM. Cells. 2020;9(10):2310. doi:10.3390/cells9102310 18. Arber DA, Orazi A, Hasserjian RP, et al. Blood. 2022;140(11):1200-1228. doi:10.1182/blood.2022015850 19. Huber S, Baer C, Hutter S, et al. Blood. 2022;140(Supplement 1):555-556. doi:10.1182/blood-2022-162326 20. Arber DA, Orazi A, Hasserjian R, et al. Blood. 2016;127(20):2391-2405. doi:10.1182/blood-2016-03-643544 21. Zeidan AM, Pollyea DA, Garcia JS, et al. Blood. 2019;134(Supplement_1):565-565. doi:10.1182/blood-2019-124994 22. DiNardo CD, Jabbour E, Ravandi F, et al. Leukemia. 2016;30(4):980-984. doi:10.1038/leu.2015.211 23. Thol F, Weissinger EM, Krauter J, et al. Haematologica. 2010;95(10):1668-1674. doi:10.3324/haematol.2010.025494 24. Medeiros BC, Fathi AT, DiNardo CD, Pollyea DA, Chan SM, Swords R. Leukemia. 2017;31(2):272-281. doi:10.1038/leu.2016.275 25. Testa U, Castelli G, Pelosi E. Cancers. 2020;12(9):2427. doi:10.3390/cancers12092427 26. Makishima H, Yoshizato T, Yoshida K, et al. Nat Genet. 2017;49(2):204-212. doi:10.1038/ng.3742 27. Molenaar RJ, Thota S, Nagata Y, et al. Leukemia. 2015;29(11):2134-2142. doi:10.1038/leu.2015.91
